Congressional Justification FY 2024
DEPARTMENT OF HEALTH AND HUMAN SERVICES
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health (NCCIH)
FY 2024 Budget Table of Contents
- Director’s Overview
- Major Changes in the Budget Request
- Budget Mechanism Table
- Appropriations Language
- Summary of Changes
- Budget Graphs
- Organization Chart
- Budget Authority by Activity Table
- Justification of Budget Request
- Appropriations History
- Authorizing Legislation
- Amounts Available for Obligation
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
General Notes
1. FY 2023 Enacted levels cited in this document include the effects of the FY 2023
HIV/AIDS transfer, as shown in the Amounts Available for Obligation table.
2. Detail in this document may not sum to the subtotals and totals due to rounding.
Director’s Overview

Helene Langevin, M.D.
Director, NCCIH
The mission of the National Center for Complementary and Integrative Health (NCCIH) is to define, through rigorous scientific investigation, the fundamental mechanisms, usefulness, and safety of complementary and integrative health approaches and their roles in improving health and health care.
Americans spend approximately $30.2 billion per year on complementary health treatments, practices, and products.1 This diverse group of health practices includes nutritional, psychological, and physical approaches. These include natural products, such as dietary supplements, plant-based products, and probiotics, as well as mind and body approaches, such as yoga, massage therapy, meditation, mindfulness-based stress reduction, spinal manipulation, and acupuncture. These treatment and self-care options are typically used in conjunction with conventional medicine to promote health and well-being, manage symptoms of a disease or condition, and alleviate side effects of medications. Integrative health care seeks to bring conventional and complementary approaches together in a safe, coordinated way with the goal of improving clinical care for patients, restoring health, promoting resilience, and preventing disease. Recently, NCCIH expanded its definition of integrative health to include whole person health, which emphasizes integration—not only of complementary and conventional care, but also physiological systems, such that an individual is viewed as a whole, rather than a collection of parts. Whole person health also emphasizes the integration of self-care and nonpharmacologic interventions to promote and restore health.
During the last few years, NCCIH has invested in a variety of efforts, including to expand its research portfolio and continue support for the National Institutes of Health (NIH)–U.S. Department of Defense (DoD)–U.S. Department of Veterans Affairs (VA) Pain Management Collaboratory. Recently, the NIH-DoD-VA Pain Management Collaboratory awarded a grant to test the effectiveness of a telecollaborative care intervention for chronic pain among rural veterans. This type of intervention is needed because despite increased availability of resources for chronic pain, veterans living in rural areas have poor access to these services and must attempt to navigate multiple health systems to receive comprehensive treatment, often resulting in poor clinical outcomes. If the results of this multisite study are significant, it will lead to improved care across the VA nationally.
As a responsible steward of resources, we are highly selective and yet support a broad range of scientifically meritorious basic, mechanistic, clinical, and translational research. We focus on areas with the greatest impact by prioritizing research topics that show scientific promise and are amenable to rigorous scientific inquiry. We strive to invest in research that will drive new discoveries and may lead to improved public health and health care. The following are some of our recent efforts to ensure general health and prevent and/or manage symptoms of disease of the whole person throughout their lifetime.
1Expenditures on complementary health approaches: United States, 2012. National Health Statistics Reports. No. 95, 2016. PMID: 2735222.
Ensuring health at all stages of life for all people
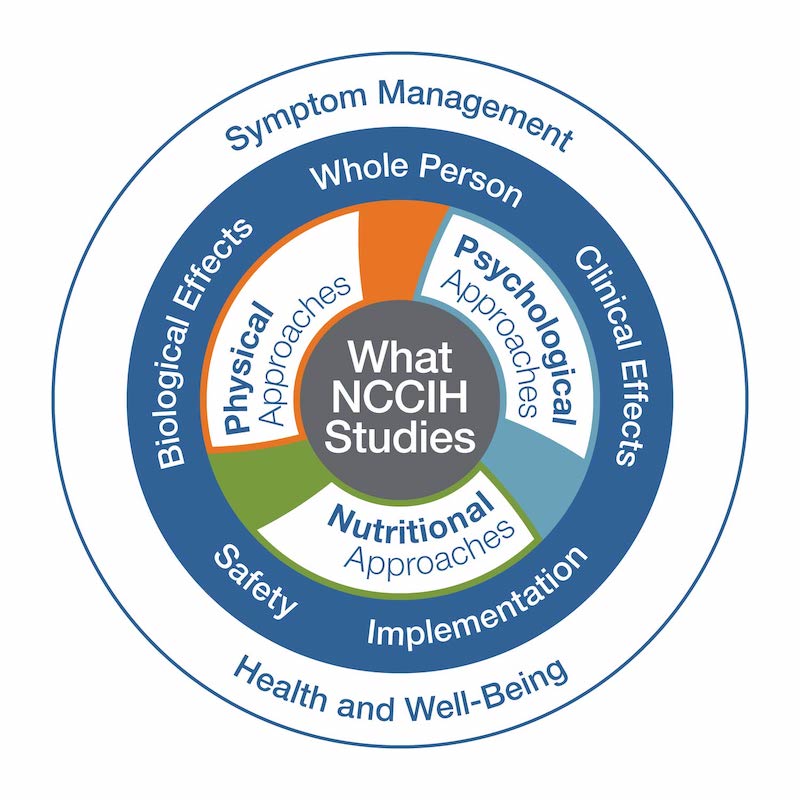
NCCIH supports research on the use of complementary and integrative health approaches to manage symptoms of disease as well as ensuring, maintaining, and restoring health and well-being of the whole person throughout their lifetime. Whole person health is the central component of NCCIH’s most recent strategic plan and is defined as empowering individuals, families, communities, and populations to improve their health in multiple interconnected domains: biological, behavioral, social, and environmental. By deepening our scientific understanding of the connections that exist across domains of human health, we can better understand how conditions interrelate, define multicomponent interventions that address these problems, and improve how we support patients through the full continuum of their health experience, including the return to health.
In one effort to expand research on whole person health, NCCIH is helping to lead a new NIH Common Fund program called Bridge to Artificial Intelligence (Bridge2AI). The Bridge2AI program brings technological and biomedical experts together with social scientists and humanists to generate new flagship biomedical and behavioral datasets that are ethically sourced, trustworthy, well-defined, and accessible. This is a critical step toward expanding the use of artificial intelligence (AI) in biomedical and behavioral research. Among the exciting projects that the program is supporting is one dedicated to better understanding the factors that promote good health and health restoration. This project will focus on type 2 diabetes and explore the interconnections across different bodily systems as it relates to health restoration. It represents a highly complex research question that will generate a massive amount of data that could only be interpretable using AI. The Bridge2AI initiative is a vital step toward unlocking the power of AI, and the inclusion of this project will help the research community build essential bridges to good health.
Psychological and social factors have major impacts on health promotion, restoration, and disease prevention at all stages of life. Stress is a prime example of this, and stress management is an important area of research supported by NCCIH. Stress is a physical and emotional reaction that people experience as they encounter challenges in life. Occasional stress induces normal coping mechanism. However, long-term stress may contribute to or worsen a range of health problems including asthma, digestive disorders, headaches, sleep disorders, depression, and anxiety. In addition to supporting research on how complementary and integrative health practices can help manage stress, NCCIH is working to bring awareness about the hazards of stress and the importance of stress management through its new “Press Reset on Stress” campaign. This effort includes a set of materials focused on identifying and managing stress. Managing stress is important for physical health, as well as mental and emotional well-being. NCCIH is also supporting research on how complementary and integrative health practices can support and improve mental and emotional well-being and their impact on health. A recent funding announcement will expand these efforts to children’s school settings. The goal is to test the efficacy or effectiveness of complementary and integrative health approaches to promote mental, emotional, and behavioral health and prevent related disorders among youth. The secondary goal is to teach lifelong skills to children that will help manage stress and support mental and emotional well-being throughout their lifetime.
Developing targeted preventions and cures
Complementary and integrative health approaches are used to promote health and well-being, manage symptoms of disease or conditions, and alleviate side effects of medications. NCCIH supports research that evaluates the safety and effectiveness of these approaches and their potential to improve health and health care.
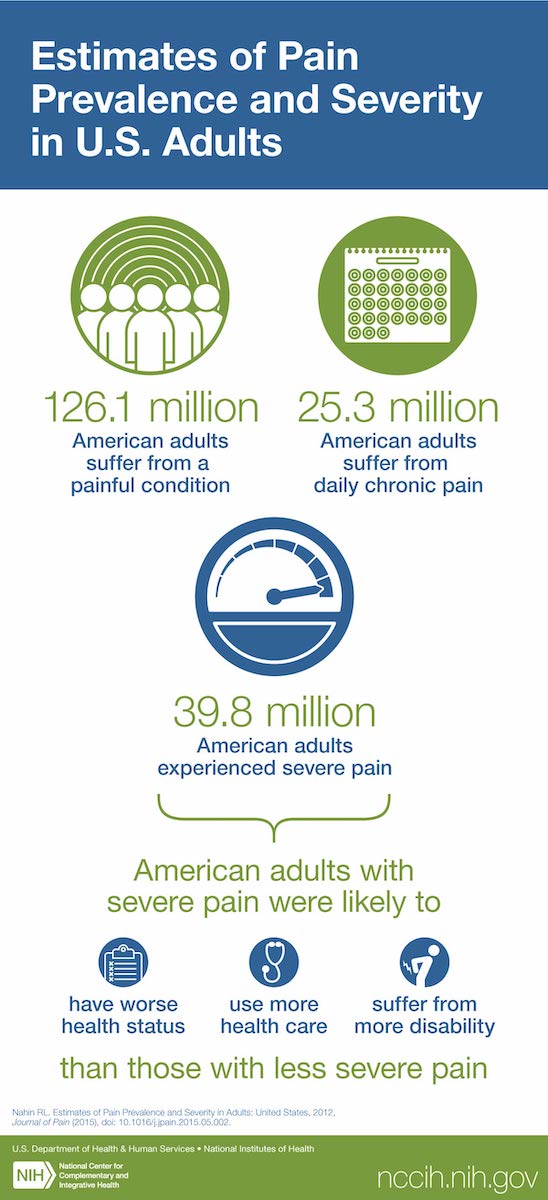
Pain and pain management is one area of focus. Pain is a major public health problem and is the most common reason why Americans use complementary and integrative health practices. Chronic pain affects millions of people, lacks effective treatments, and is a primary driver of opioid use disorders. There is an urgent need for nonaddictive approaches that can relieve or reduce pain and increase functional ability. NCCIH supports pain and pain management research from basic and mechanistic research through dissemination and implementation research. These efforts focus on understanding the basic biology of pain, identifying novel natural products for pain management, optimizing behavioral approaches to manage pain and opioid cravings, evaluating pain management options in real-world settings, and improving the implementation of evidence-based practices.
Precision probiotics is another area of research with potential health benefits that is of interest to NCCIH. Probiotics are live microorganisms found in yogurt and other fermented foods, dietary supplements, and beauty products that are suggested to have health benefits when consumed or applied to the body. These purported benefits include alleviation of gastrointestinal symptoms; strengthening of the immune system; protection against infectious diseases; prevention of metabolic disorders; improved mental health; promotion of early development; and general well-being. While probiotics have shown promise for some conditions, there are numerous types of probiotics and more research is needed to understand which probiotics are helpful, which are not, and for what conditions. Research has shown that differences in gut microbiota, diet, age, and lifestyle can impact the effects of probiotics. This has led to a growing interest in the development of individualized probiotic therapeutics for specific conditions based on an individual’s characteristics. This is referred to as precision probiotics. NCCIH sponsors a variety of research projects related to probiotics, but the Center is also interested in the emerging field of precision probiotic research. As an initial step, NCCIH hosted a workshop in 2022 to discuss issues related to precision probiotics research and potential solutions to advance the field. This event was well attended and will serve as a guide for future efforts.
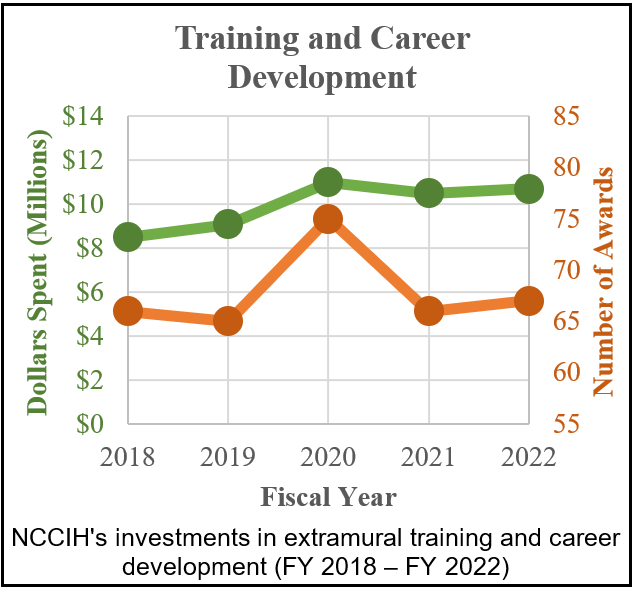
Inspiring the next generation of scientists
Researchers from many different biomedical and behavioral disciplines are key to advancing basic, mechanistic, translational, and clinical research on complementary and integrative health approaches. Over the years, NCCIH has targeted resources to attract well-trained and experienced scientists and clinicians into complementary and integrative health research, supporting their development as scientific leaders in the field. Representatives from NCCIH attend a wide variety of scientific conferences each year and meet with scientists and complementary and integrative health practitioners to inspire and support investigators. In addition, they conduct workshops at these conferences to help early-stage investigators to learn how to find NIH funding opportunities, interact with NIH staff, navigate the NIH review process, overcome career roadblocks, and plan for a successful research career. Another way NCCIH supports the next generation of scientists is through individual and institutional training opportunities. NCCIH supports a variety of training and career development activities for pre- and post-doctoral students and early career investigators. One area of particular focus is on developing clinician-scientists who have both clinical and research expertise.
The path toward becoming a clinician-scientist is not easy and may be particularly challenging for complementary and integrative health clinicians. The first issue is that complementary and integrative health clinicians may not have an opportunity to engage in research as part of their clinical training. NCCIH has worked to develop research training opportunities for these clinicians. For example, the Center supports a KL2 career development program that allows scholars with doctoral clinical complementary and integrative health degrees (i.e., Doctor of Chiropractic Medicine (D.C.), Doctor of Osteopathic Medicine (D.O.), Doctor of Naturopathic Medicine (N.D)) to collaborate with a national network of medical research institutions that can identify and test promising translational innovations. The KL2 program is specifically designed to support clinician-scientists who are at a critical point in the research career pipeline when many are lost to industry or clinical practice. Another barrier is that complementary and integrative institutions often lack the administrative resources needed to support the research of clinician-scientists. To help address this issue, NCCIH has recently released the Research Across Complementary and Integrative Health Institutions (REACH) initiative. This program will support virtual resource centers that will foster institutional partnerships between large research institutions and smaller complementary and integrative health institutions to perform the necessary administrative functions related to writing and submitting a competitive grant application and conducting research. It is expected that REACH virtual resource centers will help to enhance the research environment at integrative health clinical institutions and help to further develop clinician-scientists trained in complementary and integrative health practices.
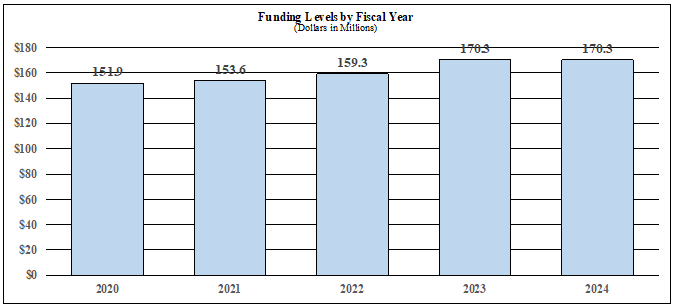
Major Changes in the Budget Request
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanisms and activity detail, and these highlights will not sum to the total change for the FY 2024 budget request for the NCCIH, which is $170.3 million, equal to the FY 2023 enacted level. Within the request level, NCCIH will pursue its highest research priorities through strategic investments and careful stewardship of appropriated funds.
Research Project Grants (-$2.4 million; total $89.9 million): NCCIH will support a total of 174 Research Project Grant (RPG) awards in FY 2024. Noncompeting RPGs will decrease by $1.5 million, and Competing RPG awards will decrease by $0.9 million.
R&D Contracts (+$0.0 million; total $12.0 million): NCCIH will continue its annual support to the National Health Interview Survey (NHIS) and other mission-supporting Research and Development Contracts.
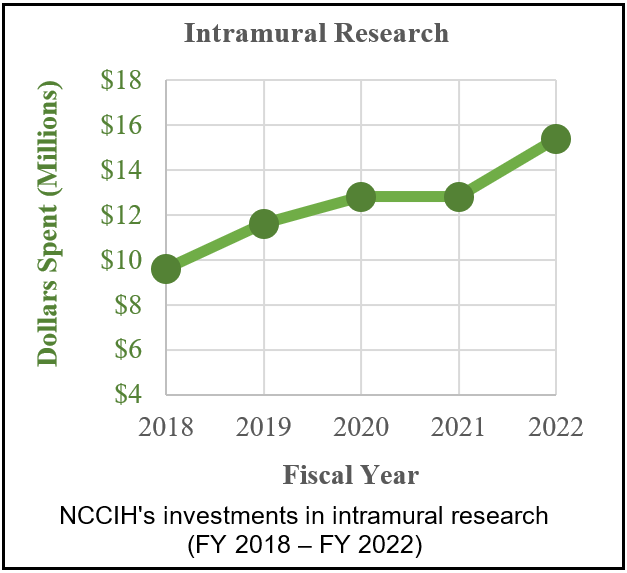
Intramural Research (+$0.4 million; total $17.0 million): NCCIH will continue to support intramural research activities, including the NIH Pain Research Center.
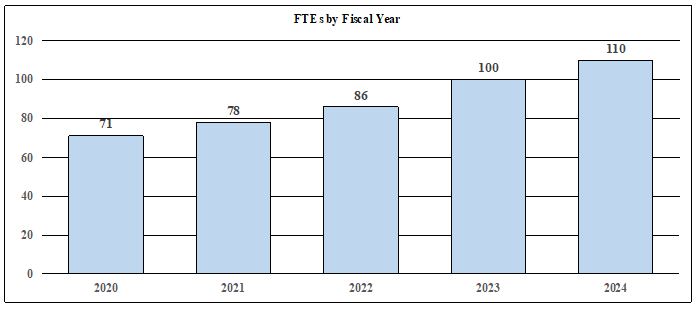
Research Management and Support (+$0.5 million; total $22.2 million): NCCIH will manage a full-time equivalent staff level of 110 and fund the costs of pay raises, benefit increases, and other inflation.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Mechanism*
(Dollars in Thousands)
| MECHANISM | FY 2022 Final | FY 2023 Enacted | FY 2024 President’s Budget | FY 2024 +/- FY 2023 CR | ||||
|---|---|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | No. | Amount | |
| Research Projects: | ||||||||
| Noncompeting | 118 | $64,866 | 118 | $63,849 | 113 | $62,329 | -5 | $-1,520 |
| Administrative Supplements | (16) | $1,481 | (6) | $600 | (6) | $600 | (0) | $0 |
| Competing: | ||||||||
| Renewal | 4 | $1,857 | 4 | $1,708 | 4 | $1,713 | 0 | $6 |
| New | 42 | $17,959 | 50 | $21,346 | 48 | $20,559 | -2 | -$786 |
| Supplements | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Subtotal, Competing | 46 | $19,815 | 54 | $23,053 | 52 | $22,273 | -2 | -$781 |
| Subtotal, RPGs | 164 | $86,162 | 172 | $87,503 | 165 | $85,201 | -7 | -$2,301 |
| SBIR/STTR | 8 | $4,440 | 9 | $4,773 | 9 | $4,739 | 0 | -$34 |
| Research Project Grants | 172 | $90,602 | 181 | $92,275 | 174 | $89,940 | -7 | -$2,335 |
| Research Centers: | ||||||||
| Specialized/Comprehensive | 1 | $2,388 | 1 | $3,410 | 2 | $3,860 | 1 | $449 |
| Clinical Research | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Biotechnology | 1 | $733 | 0 | $201 | 0 | $201 | 0 | $0 |
| Comparative Medicine | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers in Minority Institutions | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers | 2 | $3,120 | 1 | $3,612 | 2 | $4,061 | 1 | $449 |
| Other Research: | ||||||||
| Research Careers | 41 | $6,381 | 42 | $6,611 | 49 | $7,622 | 7 | $1,011 |
| Cancer Education | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Cooperative Clinical Research | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Biomedical Research Support | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Minority Biomedical Research Support | 0 | $150 | 0 | $150 | 0 | 0 | 0 | -$150 |
| Other | 20 | $9,431 | 26 | $12,538 | 26 | $12,660 | 0 | $122 |
| Other Research | 61 | $15,963 | 68 | $19,298 | 75 | $20,282 | 7 | $983 |
| Total Research Grants | 235 | $109,684 | 250 | $115,186 | 251 | $114,283 | 1 | -$903 |
| Ruth L Kirchstein Training Awards: | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 16 | $655 | 23 | $929 | 26 | $1,080 | 3 | $152 |
| Institutional Awards | 44 | $3,661 | 47 | $3,889 | 44 | $3,683 | -3 | -$206 |
| Total Research Training | 60 | $4,316 | 70 | $4,818 | 70 | $4,763 | 0 | -$55 |
| Research & Develop. Contracts | 15 | $9,603 | 11 | $11,976 | 11 | $11,976 | 0 | $0 |
| (SBIR/STTR) (non-add) | (0) | ($46) | (0) | ($48) | (0) | ($48) | (0) | ($0) |
| Intramural Research | 12 | $15,440 | 16 | $16,658 | 20 | $17,075 | 4 | $416 |
| Res. Management & Support | 74 | $20,239 | 84 | $21,639 | 90 | $22,180 | 6 | $541 |
| SBIR Admin (non-add) | ($0) | ($0) | ($0) | ($0) | ||||
| Construction | $0 | $0 | $0 | $0 | ||||
| Buildings and Facilities | $0 | $0 | $0 | $0 | ||||
| Total, NCCIH | 86 | $159,282 | 100 | $170,277 | 110 | $170,277 | 10 | $0 |
* All items in italics and brackets are non-add entries.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Appropriations Language
For carrying out section 301 and title IV of the PHS Act with respect to complementary and integrative health, [$170,384,000]$170,277,000.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Summary of Changes
(Dollars in Thousands)
| FY 2023 Enacted | $170,277 | ||||||
|---|---|---|---|---|---|---|---|
| FY 2024 President’s Budget | $170,277 | ||||||
| Net Change | $0 | ||||||
| CHANGES | FY 2023 Enacted | FY 2024 President’s Budget | Built-In Change from FY 2023 Enacted | ||||
| FTEs | Budget Authority | FTEs | Budget Authority | FTEs | Budget Authority | ||
| A. Built-in: | |||||||
| 1. Intramural Research: | |||||||
| a. Annualization of FY 2023 pay & benefits increase | $4,341 | $4,963 | $49 | ||||
| b. FY 2024 pay & benefits increase | $4,341 | $4,963 | $167 | ||||
| c. Paid days adjustment | $4,341 | $4,963 | $17 | ||||
| d. Differences attributable to change in FTE | $4,341 | $4,963 | $1,085 | ||||
| e. Payment for centrally furnished services | $2,131 | $2,165 | $34 | ||||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | $10,186 | $9,947 | $222 | ||||
| Subtotal | $1,573 | ||||||
| 2. Research Management and Support: | |||||||
| a. Annualization of FY 2023 pay & benefits increase | $15,519 | $16,755 | $171 | ||||
| b. FY 2024 pay & benefits increase | $15,519 | $16,755 | $593 | ||||
| c. Paid days adjustment | $15,519 | $16,755 | $60 | ||||
| d. Differences attributable to change in FTE | $15,519 | $16,755 | $1,136 | ||||
| e. Payment for centrally furnished services | $219 | $223 | $4 | ||||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | $5,901 | $5,202 | $122 | ||||
| Subtotal | $2,084 | ||||||
| Subtotal, Built-in | $3,657 | ||||||
| CHANGES | FY 2023 Enacted | FY 2024 President’s Budget | Program Change from FY 2023 Enacted | |||
|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | |
| B. Program: | ||||||
| 1. Research Project Grants: | ||||||
| a. Noncompeting | 118 | $64,449 | 113 | $62,929 | -5 | -$1,520 |
| b. Competing | 54 | $23,053 | 52 | $22,273 | -2 | -$781 |
| c. SBIR/STTR | 9 | $4,773 | 9 | $4,739 | 0 | -$34 |
| Subtotal, RPGs | 181 | $92,275 | 174 | $89,940 | -7 | -$2,335 |
| 2. Research Centers | 1 | $3,612 | 2 | $4,061 | 1 | $449 |
| 3. Other Research | 68 | $19,298 | 75 | $20,282 | 7 | $983 |
| 4. Research Training | 70 | $4,818 | 70 | $4,763 | 0 | -$55 |
| 5. Research and development contracts | 11 | $11,976 | 11 | $11,976 | 0 | $0 |
| Subtotal, Extramural | $131,980 | $131,022 | -$957 | |||
| 6. Intramural Research | 16 | $16,658 | 20 | $17,075 | 4 | -$1,157 |
| 7. Research Management and Support | 84 | $21,639 | 90 | $22,180 | 6 | -$1,543 |
| 8. Construction | $0 | $0 | $0 | |||
| 9. Buildings and Facilities | $0 | $0 | $0 | |||
| Subtotal, Program | 100 | $170,277 | 110 | $170,277 | 10 | -$3,657 |
| Total built-in and program changes | $0 | |||||
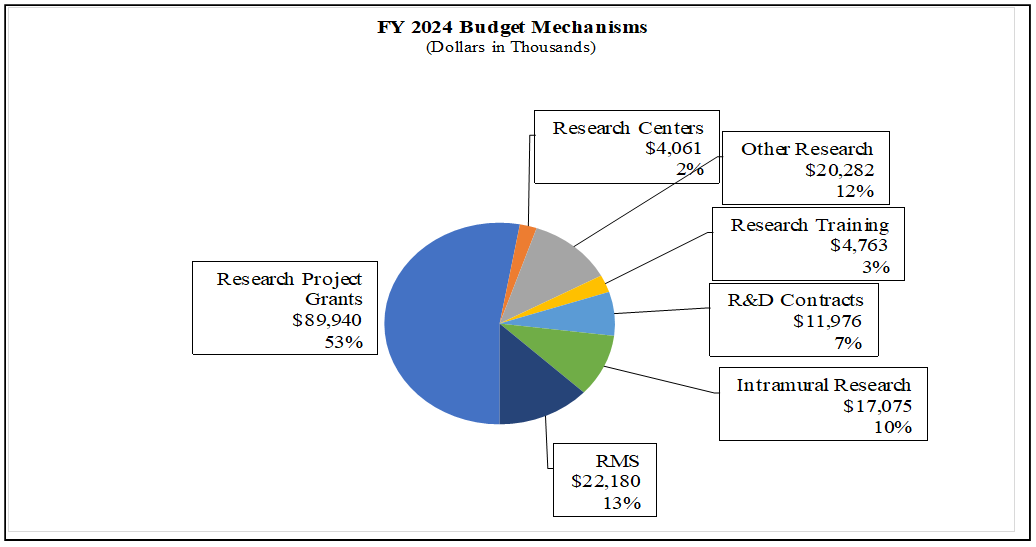
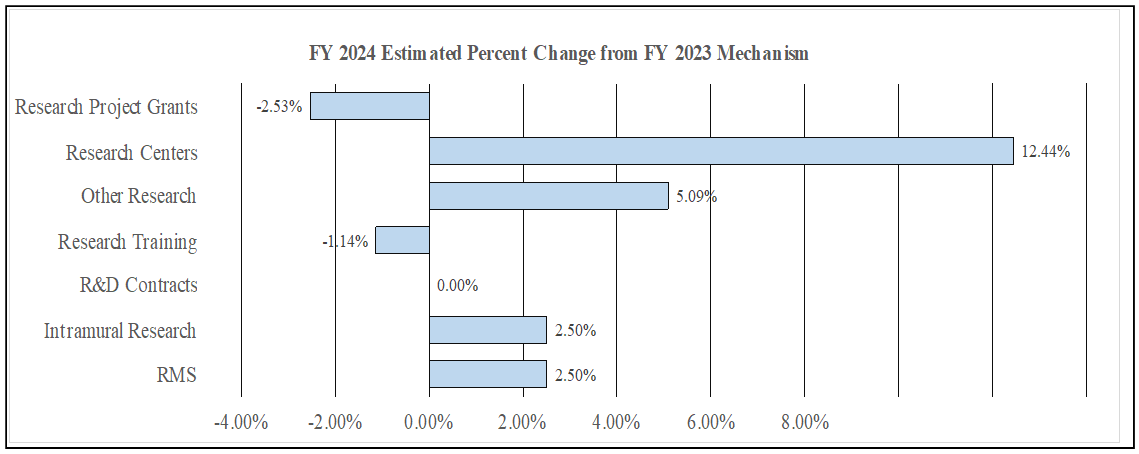
Budget Graphs
History of Budget Authority and FTEs:
Distribution by Mechanism:
Change by Selected Mechanisms:
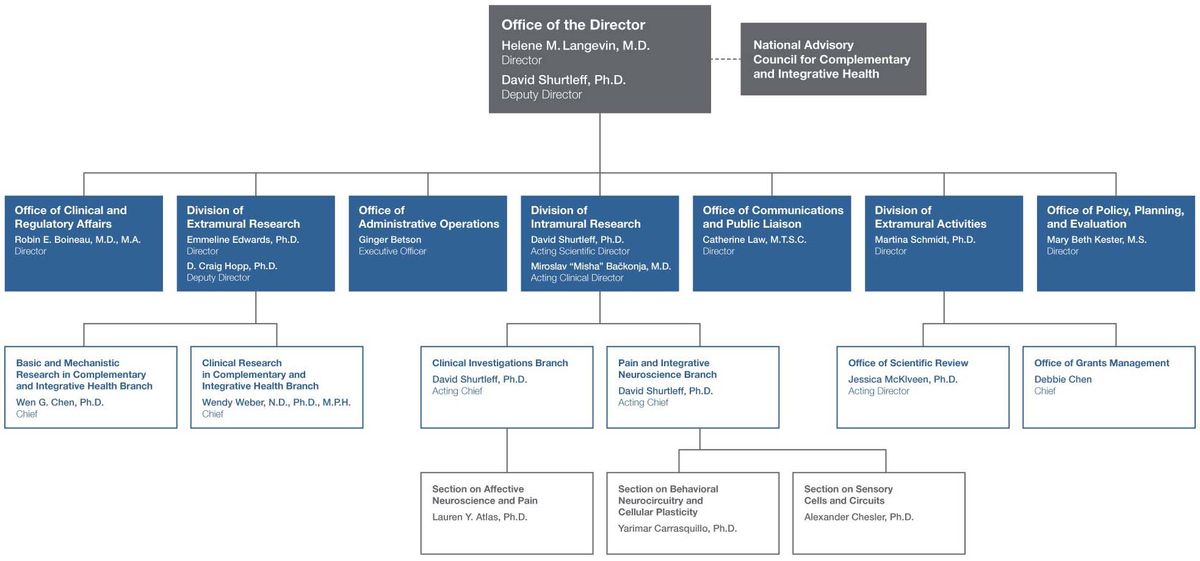
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Organizational Chart
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Authority by Activity*
(Dollars in Thousands)
| FY 2022 Final | FY 2023 Enacted | FY 2024 President’s Budget | FY 2024 +/- FY2023 Enacted | |||||
|---|---|---|---|---|---|---|---|---|
| Extramural Research | FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount |
* Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | ||||||||
| Detail | ||||||||
| Clinical Research-Non Pain | $28,766 | $30,304 | $29,519 | -$786 | ||||
| Basic Research-Non Pain | $41,288 | $43,496 | $42,368 | -$1,128 | ||||
| Extramural Pain and Pain Management | $42,851 | $46,751 | $46,751 | $0 | ||||
| Extramural Research Training and Capacity Building | $10,697 | $11,429 | $12,385 | $956 | ||||
| Subtotal, Extramural | $123,603 | $131,980 | $131,022 | -$957 | ||||
| Intramural Research | 12 | $15,440 | 16 | $16,658 | 20 | $17,075 | 4 | $416 |
| Research Management & Support | 74 | $20,239 | 84 | $21,639 | 90 | $22,180 | 6 | $541 |
| TOTAL | 86 | $159,282 | 100 | $170,277 | 110 | $170,277 | 10 | $0 |
National Center for Complementary and Integrative Health
Justification of Budget Request
Authorizing Legislation: Section 301 and Title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2022 Final | FY 2023 Enacted | FY 2024 President’s Budget | FY 2024 +/- FY 2022 | |
|---|---|---|---|---|
| BA | $159,282,000 | $170,277,000 | $170,277,000 | $0 |
| FTE | 86 | 100 | 110 | 10 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Overall Budget Policy: The FY 2024 President’s Budget request for NCCIH is $170.3 million, the same as the FY 2023 enacted level.
Program Descriptions and Accomplishments
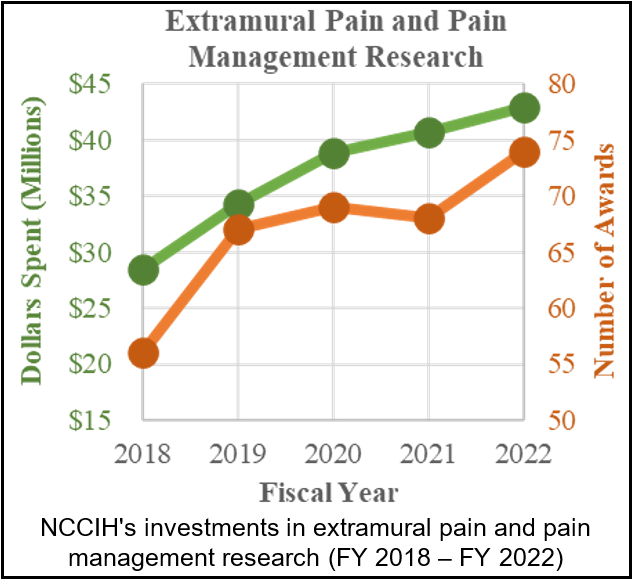
Extramural Pain and Pain Management Research

Pain is a major public health problem and is the most common reason why Americans use complementary and integrative health practices. As a result, NCCIH has also made pain management a major emphasis in its research efforts. The NCCIH extramural pain and pain management research program supports basic and clinical research on the biological basis of pain and the development, evaluation, and implementation of complementary and integrative pain management techniques. The following is an example of research supported by this program.
Researchers from Michigan State University and Cincinnati Children’s Hospital Medical Center recently found that youth with functional abdominal pain disorders (FAPDs) have distinctive patterns of brain connectivity that could support the development of biomarkers and inform new treatment approaches. FAPDs, such as irritable bowel syndrome, are among the most common pain conditions affecting youth. They are thought to result from abnormal interactions between the brain and the gut, but the exact mechanisms of the interactions are poorly understood, diagnosis of the conditions is difficult, and treatment is challenging. This recently published study used functional magnetic resonance imaging (fMRI) to evaluate brain structure and function. The focus of the study was on the amygdala because this brain region is associated with visceral pain (pain in or around the internal organs) and negative affect (emotional distress). The study found that the brains of youth with FAPDs function differently than those of healthy youth, with distinctive patterns of amygdala connectivity. Understanding these patterns may help researchers develop biomarkers that could aid in identifying FAPDs and distinguishing them from other conditions. The investigators noted that there are limited evidence-based treatments currently available for FAPDs and that the results of their study may inform the development and testing of better treatment approaches.2
2Cunningham NR, et al. Amygdalar functional connectivity during resting and evoked pain in youth with functional abdominal pain disorders. Pain. 2022.
Budget Policy:
The FY 2024 President’s Budget request for extramural pain and pain management research is $46.8 million, unchanged from the FY 2023 Enacted level.
Efforts To Advance Myofascial Pain Research
Myofascial pain is a type of pain that originates from muscles and/or soft tissues called fascia. Very little is known about myofascial pain, but it is likely an important component of many severe and chronic pain conditions such as chronic low back pain, temporomandibular disorders, chronic neck and shoulder pain, and headaches. However, knowledge regarding the contribution of myofascial tissues—especially fascia and the interactions between fascia, muscles, and nerves—to many pain types remains lacking. An estimated 30 to 50 percent of patients diagnosed with musculoskeletal pain also have myofascial pain. The field of musculoskeletal pain research focuses on the skeletal system (bones, joints, intervertebral discs) and central nervous system (brain and spinal cord) while the effects of the myofascial remain largely unexplored. Many chronic musculoskeletal pain patients do not respond to surgery (targeting joint and other skeletal pathology) or develop significant side effects from pharmacotherapy, including nonopioid and opioid analgesics (targeting the nervous system). It is hypothesized that these patients’ persistent pain is due to ineffective treatment of the myofascial component of their pain. Evidence for treatment of myofascial pain is limited, and clinicians currently lack objective guidance on how to treat pain conditions with myofascial origin. In 2020, NCCIH partnered with nine other NIH Institutes, Centers, and Offices as well as the NIH Helping to End Addiction Long-term (HEAL) Initiative to host a workshop with experts in musculoskeletal pain research. It was suggested that the field of myofascial pain has been hindered by a lack of objective methods to evaluate myofascial tissues or biomarkers to study myofascial tissue pathophysiology. In 2022, NCCIH, the NIH HEAL Initiative, and other NIH partners released a new funding initiative in an effort to address this gap. The funding opportunity sought to support the development of innovative quantitative imaging and other relevant biomarkers of myofascial tissues for pain management. This initiative ultimately funded seven awards that will contribute to advancing research on myofascial tissues and their role in pain. Since a substantial proportion of patients with low-back, neck, shoulder, or temporomandibular pain or headache and migraine may have myofascial contributions, research on myofascial pain may help develop novel therapies for these pain conditions.
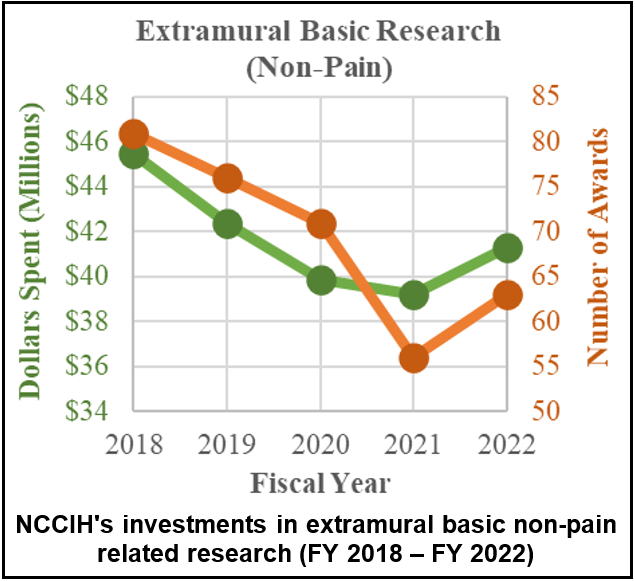
Extramural Basic Research (Non-Pain)

The NCCIH extramural basic research program seeks to understand the fundamental science of complementary health approaches such as their biology, physiology, physical, chemical, and behavioral properties. This includes research on basic physiological and pathophysiological mechanisms relevant to complementary and integrative health. It also includes identifying and understanding the active components of a complementary health approach and how these components produce effects. Depending on the question, basic and mechanistic studies may be performed in the laboratory, in experimental models, or with research participants. NCCIH is also energizing the research community to overcome the methodologic and technologic obstacles hindering basic research on natural products and nonpharmacologic therapies, as well as encouraging the incorporation of cutting-edge technologies to monitor and enhance these interventions. The following is an example of research supported by this program.
Researchers from Harvard Medical School and Brigham and Women’s Hospital in Boston and Monash University in Clayton, Victoria, Australia investigated the impact of diet on the human gut bacteria Bacteroidesfragilis (B. fragilis), the metabolites it produces, and its effects on host immune regulation. It is known that microbial metabolites produced by gut microbes like B. fragilis play critical roles in host immune development and health, but little is known about the exact mechanisms responsible for these effects. The researchers of this study sought to explore these mechanisms. They first investigated the effect of specific amino acids obtained through diet on a group of lipids produced by B. fragilis. They found that specific amino acids affected the structure of B. fragilis produced lipids. They then looked at how the structure of these lipids affected the function of colonic natural killer T (NKT) cells, a type of gut immune cell. NKT cells are known to react to diverse lipid antigens from microbes and play an important role in the regulation of immunity to pathogens and/or tumors and in autoimmune and/or metabolic disorders. The researchers in this study identified distinct types of bacterial lipid structures for NKT-induced anti-inflammatory responses. Taken together, the results of this study suggested that changes in one component of a host animal’s nutrition can directly influence the structure of small molecules produced by intestinal bacteria and that these modifications can influence immune regulation in the host. These findings may inform the future development of dietary, probiotic, or small molecule interventions for diseases that are influenced by colonic NKT cells, such as inflammatory bowel diseases.3
3Oh SF, et al. Host immunomodulatory lipids created by symbionts from dietary amino acids. Nature. 2021.
Budget Policy:
The FY 2024 President’s Budget request for extramural basic research (non-pain) is $42.4 million, a decrease of $1.1 million compared with the FY 2023 enacted level.
NCCIH-Supported Public-Private Partnership Helps to Advance Natural Smoking Cessation Aid
Illnesses and deaths linked to tobacco smoking are a huge public health problem in the United States and worldwide. Although treatments such as counseling and medication are available to help people stop smoking, research indicates that these treatments are not always available or successful for every patient, and that an individualized approach is desirable. Giving smokers additional treatment options may increase the likelihood that they will quit successfully. The natural product cytisine (also known as cytisinicline) has been used as a smoking cessation aid in some central and eastern European countries for decades. Despite promising results from clinical trials conducted outside the United States, cytisine has not yet been approved for use in the United States. In 2015, NCCIH started a public-private partnership with Achieve Life Sciences, Inc., to advance clinical trials of cytisine in the United States. This approximately $1.7 million investment allowed Achieve Life Sciences, Inc. to conduct the preclinical safety and toxicology studies needed to apply for an Investigational New Drug (IND) application with the U.S. Food and Drug Administration (FDA). In August 2017, Achieve Life Sciences, Inc. submitted, and the FDA approved, an IND for cytisine allowing it to proceed with clinical trials in the United States. In 2022, Achieve Life Sciences, Inc. announced promising results for its Phase III clinical trials. They found that participants taking cytisine were six to eight times more likely to quit smoking than the control group. In addition, there were no serious adverse events. These results suggest that cytisine is a safe and effective smoking cessation aid. In 2023, if a second wave of Phase III clinical trials is successful, Achieve Life Sciences, Inc. plans to file a New Drug Application (NDA) with the FDA. This is the next step in the process of bringing cytisine to the U.S. market. If the FDA approves the NDA and authorizes it for use as a smoking cessation aid, it will give smokers an additional tool to help them quit smoking. This will, in turn, help reduce the number of lives lost or impaired from tobacco smoking and nicotine addiction.
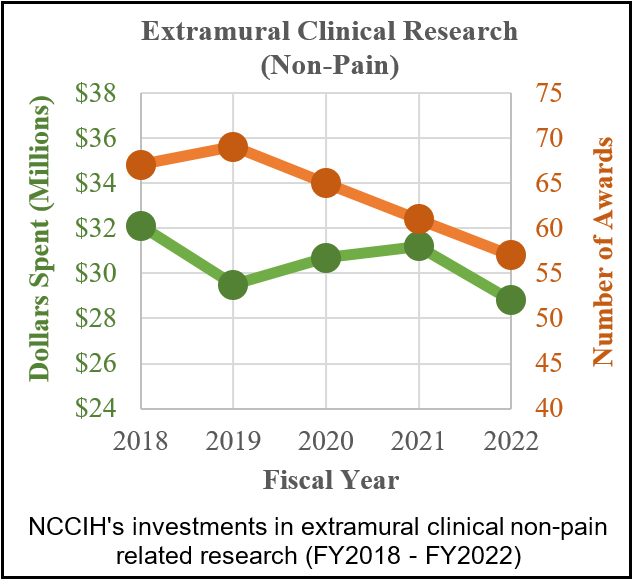
Extramural Clinical Research (Non-Pain)

The NCCIH extramural clinical research program supports trials of complementary and integrative health approaches, including early- and mid-phase testing to assess biological signatures of these interventions in humans (and replication of these effects), define appropriate dosage, refine the components and mode of intervention delivery, determine optimal frequency or duration of the intervention, assess feasibility, and enhance adherence. The Center also supports later stage full-scale efficacy or effectiveness trials when the evidence base is sufficient to justify them. When interventions have been found effective, the Center supports pragmatic or implementation trials to integrate interventions into health care systems. The following is an example of research supported by this program.
Researchers from the EMMES Corporation; University of Wisconsin, Madison; Harvard Medical School; and the National Eye Institute evaluated 10 years of data from the Age-Related Eye Disease Study 2 (AREDS2) clinical trial and found that substituting lutein and zeazanthin for beta-carotene, which had been used in the previous AREDS1 study, slowed the progression of age-related macular degeneration (AMD), increased the supplement’s effectiveness, and reduced the risk of lung cancer in smokers associated with beta-carotene. The AREDS1 clinical trial, launched in 1996, showed that a dietary supplement formula of 500 milligrams (mg) vitamin C, 400 international units vitamin E, 2 mg copper, 80 mg zinc, and 15 mg beta-carotene could significantly slow the progression of AMD from moderate to late disease. However, two concurrent but unrelated studies revealed that people who smoked and took beta-carotene supplements had a higher risk of developing lung cancer. The AREDS2 clinical trial, which began in 2006, compared a formula with 10 mg lutein and 2 mg zeaxanthin in place of beta-carotene with the original beta-carotene formulation. This new analysis contacted 3,883 of the original 4,203 AREDS2 participants to evaluate whether their AMD had progressed and whether they had been diagnosed with lung cancer. The follow-up study showed that beta-carotene nearly doubled the risk of lung cancer for those who had ever smoked, and there was no increased risk of lung cancer in those receiving lutein and zeaxanthin. Furthermore, after 10 years, the group originally assigned to receive lutein and zeaxanthin had an additional 20 percent reduced risk for late AMD progression compared to those who received beta-carotene. The researchers who conducted the new analysis concluded that lutein and zeaxanthin are an appropriate replacement for beta-carotene that is safe and effective for long-term use4. The AREDS2 formulation is a commercially available supplement.
4Chew EY, et al. Long-term outcomes of adding lutein/zeaxanthin and ω-3 fatty acids to the AREDS supplements on age-related macular degeneration progression: AREDS2 Report 28.JAMA Ophthalmology. 2022.
Budget Policy:
The FY 2024 President’s Budget request for extramural clinical research (non-pain) is $29.5 million, a decrease of $0.8 million compared with the FY 2023 enacted level.
Intramural Research

The NCCIH Division of Intramural Research (DIR) conducts basic, clinical, and translational research focusing on the role of the nervous system, other physiological systems, and psychosocial factors in perceiving, modifying, and managing pain, with the long-term goal of improving clinical management of chronic pain through the integration of pharmacologic and nonpharmacologic approaches. Projects include investigating the role of the brain in pain processing and control and how factors such as emotion, attention, environment, and genetics affect pain perception. The program includes research that explores how chronic pain produces changes in the brain that can modify how the brain reacts to pain medications like opioids. The program both engages and leverages the exceptional basic and clinical research talent and resources of other neuroscience and neuroimaging efforts within the NIH intramural community. The NCCIH DIR provides a rich environment for the training and development of clinical and basic scientists. The following is an example of research supported by this program.
NCCIH researchers evaluated gender differences in test-retest reliability of pain sensitivity in humans and found that acute pain tolerance is more consistent over time in women than men. Many researchers exclude women from pain studies because they assume that hormonal changes in women lead to more variability over time and less reliability in ratings of pain.This study sought to test this assumption. This is important because excluding women or any subpopulation from research produces knowledge that is not necessarily applicable to them. For example, there are striking sex/gender differences in the prevalence, progression, and outcome of numerous conditions, including diabetes, obesity, cardiovascular diseases, substance abuse disorders, depression and brain disorders, infectious diseases, lupus and other autoimmune diseases, and cancer. In this study, researchers measured the pain sensitivity of 171 healthy volunteers who completed a pain test at multiple visits. Researchers evaluated the test-retest reliability of three pain measures: pain threshold, pain tolerance, and the association between temperature and pain. Female participants had higher test-retest reliability than male participants on all three pain measures. Differences were especially strong in pain tolerance — even though male participants had higher tolerance, female participants were less variable across visits. The findings also showed that pain threshold and pain tolerance were moderately reliable measures (consistent across visits) and remained relatively stable regardless of gender, testing environment, and duration between visits. Results for this study showed that women have higher test-retest reliability (a measure of consistency across measurements) on thermal (temperature-related) pain measures than men, disproving the assumption used to justify including only men in pain research. Understanding whether measures of pain are reliable is critical for evaluating their usefulness in assessing and diagnosing pain. Participation in pain research has historically been limited to men; however, the findings from this study support the inclusion of women in pain research and illustrate the need to test assumptions in research models.5
5Amir C, et al. Test-retest reliability of an adaptive thermal pain calibration procedure in healthy volunteers.Journal of Pain. 2022.
Budget Policy:
The FY 2024 President’s Budget request for intramural research is $17.0 million, an increase of $0.4 million compared with the FY 2023 enacted level.
Extramural Research Training and Capacity Building

Improving the capacity of the field to carry out rigorous research on complementary and integrative health approaches is a priority for NCCIH. To increase the number, quality, and diversity of investigators conducting this research, NCCIH supports a variety of training and career development activities for pre- and post-doctoral students, and early career investigators. NCCIH’s training strategies include innovative approaches that incorporate an understanding of the wide variety of modalities and specialization represented in complementary and integrative health fields. In addition to scientists trained in key biomedical and behavioral research disciplines, the Center has opportunities for clinician-scientists, including conventionally trained physicians, complementary health practitioners, and other health care professionals (e.g., clinical psychologists and nurses) who conduct research across a wide range of complementary and integrative health approaches, including a program to support research training for clinicians through the National Clinical and Translational Science Awards (CTSA) Program. NCCIH also has career development funding opportunities for individuals from groups who are underrepresented in scientific research (e.g., racial, and ethnic minority populations) and are interested in careers in complementary and integrative health research. In addition to these funding initiatives, NCCIH supports workshops to help students and fellows connect to NIH funding opportunities, understand how to interact with NIH staff to develop research proposals, navigate the NIH peer-review process successfully, develop resilience to overcome career roadblocks, and develop plans for a successful research career. The following is an example of recently published results from a supported investigator.
Researchers at Oregon Health & Science University found that practicing yogic breathing affects an individual’s cerebrospinal fluid (CSF) dynamics—the movement, flow, and circulation of the CSF. CSF is a type of fluid compartment around the brain and spinal cord that serves as a cushion for these organs. CSF distributes nutrients and hormones and, along with interstitial fluid (ISF, the fluid found in the spaces around cells), helps the central nervous system to remove metabolic waste. Understanding how the CSF moves and exchanges with ISF is of high importance for Alzheimer’s and other diseases of the nervous system. Previous research discovered that CSF flow oscillations during the nonrapid eye movement stage of sleep are deeper and slower than the oscillations during wakefulness. This change in CSF dynamics that occurs during sleep may increase the rate at which the brain clears itself of waste because of increased exchange between the CSF and ISF. Researchers in this study hypothesized that a similar alteration in CSF flow oscillations and CSF-ISF exchange may occur during deep yogic breathing. To test their hypothesis, the researchers used magnetic resonance imaging (MRI) to measure and compare the CSF velocities during yogic breathing and regular breathing. Researchers found that participants experienced a 16 to 28 percent increase in the power and velocity of the CSF flow in the skull during yogic breathing when compared to spontaneous breathing. Of the yogic breathing conditions, deep abdominal breathing led to the most statistically significant increase of CSF oscillation. Moreover, heart pulsation was shown to be the primary driver of the CSF movements during all the breathing conditions, except for deep abdominal breathing, when there was a similar contribution of power from both respiration and heart pulsation. This study suggests that respiration could be a primary driver of CSF dynamics, depending on the form of breathing an individual is practicing. The researchers noted that the next step is to see how long-term yogic breathing training could affect the CSF dynamics, and therefore central nervous system health.6
6Yildiz S, et al. Immediate impact of yogic breathing on pulsatile cerebrospinal fluid dynamics. Scientific Reports. 2022.
Budget Policy:
The FY 2024 President’s Budget request for extramural research training and capacity is $12.4 million, an increase of $1.0 million compared with the FY 2023 enacted level.
Research Management Support (RMS)
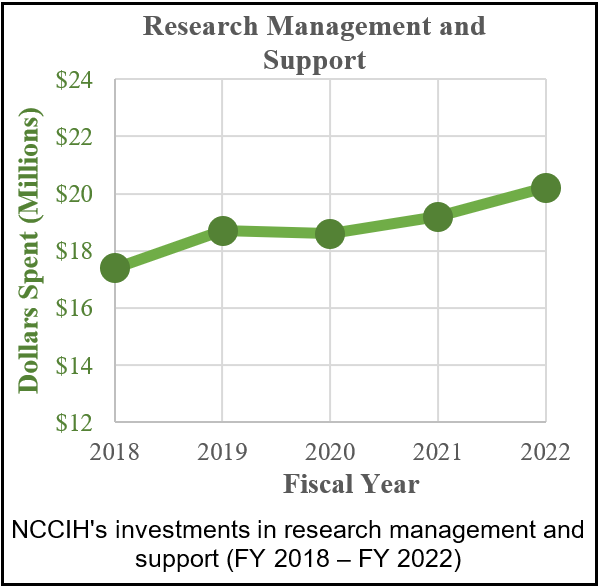
Through its RMS activities, NCCIH provides administrative, budgetary, information technology, logistical, and scientific support in the review, award, monitoring, and management of research grants, training awards, and contracts. RMS functions also encompass strategic planning, coordination, and evaluation of programs. The Center uses Qlik Sense to compile interactive reports and enhanced dashboards to provide NCCIH leadership with trend data and performance indicators to ensure responsible stewardship of public funds. In addition to these activities, NCCIH disseminates objective, evidence-based information to the public, scientists, and health care providers to help them make informed decisions about the use of complementary and integrative health practices. All information is freely available on the NCCIH website (nccih.nih.gov) or through the NCCIH Information Clearinghouse.
Budget Policy:
The FY 2024 President’s Budget request for RMS is $22.2 million, an increase of $0.5 million compared with the FY 2023 enacted level.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation | ||||
|---|---|---|---|---|---|---|---|---|
1 Budget Estimate to Congress includes mandatory financing. | ||||||||
| 2015 | $124,509,000 | $124,681,000 | ||||||
| Rescission | $0 | |||||||
| 2016 | $127,521,000 | $127,585,000 | $130,162,000 | $130,789,000 | ||||
| Rescission | $0 | |||||||
| 20171 | $129,941,000 | $134,549,000 | $136,195,000 | $134,689,000 | ||||
| Rescission | $0 | |||||||
| 2018 | $101,793,000 | $136,741,000 | $139,654,000 | $142,184,000 | ||||
| Rescission | $0 | |||||||
| 2019 | $130,717,000 | $143,882,000 | $146,550,000 | $146,473,000 | ||||
| Rescission | $0 | |||||||
| 2020 | $126,081,000 | $153,632,000 | $154,695,000 | $151,740,000 | ||||
| Rescission | $0 | |||||||
| 2021 | $138,167,000 | $153,045,000 | $156,823,000 | $154,162,000 | ||||
| Rescission | $0 | |||||||
| 2022 | $184,323,000 | $185,295,000 | $184,249,000 | $159,365,000 | ||||
| Rescission | $0 | |||||||
| 2023 | $183,368,000 | $164,395,000 | $174,305,000 | $170,384,000 | ||||
| Rescission | $0 | |||||||
| 2024 | $170,277,000 | |||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2023 Amount Authorized | FY 2023 Enacted | 2024 Amount Authorized | FY 2024 President’s Budget | |||
|---|---|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | Indefinite | ||||
| $170,277,000 | $170,277,000 | |||||||
| National Center for Complementary and Integrative Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total, Budget Authority | $170,277,000 | $170,277,000 | ||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Amounts Available for Obligation1
(Dollars in Thousands)
| Source of Funding | FY 2022 Final | FY 2023 Enacted | FY 2024 President’s Budget |
|---|---|---|---|
| Appropriation | $159,365 | $170,384 | $170,277 |
| Mandatory Appropriation: (non-add) | |||
| Type 1 Diabetes | ($0) | ($0) | ($0) |
| Other Mandatory financing | ($0) | ($0) | ($0) |
| Secretary's Transfer | $0 | $0 | $0 |
| Subtotal, adjusted appropriation | $159,365 | $170,384 | $170,277 |
| OAR HIV/AIDS Transfers | -$83 | -$107 | $0 |
| Subtotal, adjusted budget authority | $159,282 | $170,277 | $170,277 |
| Unobligated balance, start of year | $0 | $0 | $0 |
| Unobligated balance, end of year (carryover) | $0 | $0 | $0 |
| Subtotal, adjusted budget authority | $159,282 | $170,277 | $170,277 |
| Unobligated balance lapsing | -$5 | $0 | $0 |
| Total obligations | $159,277 | $170,277 | $170,277 |
| 1 Excludes the following amounts (in thousands) for reimbursable activities carried out by this account: FY 2022 — $1,570 FY 2023 — $1,352 FY 2024 — $1,406 | |||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Authority by Object Class1
(Dollars in Thousands)
| FY 2023 Enacted | FY 2024 President’s Budget | FY 2024 +/- FY 2023 | |
|---|---|---|---|
| Total compensable workyears: | |||
| Full-time equivalent | 100 | 110 | 10 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $0 | $0 | $0 |
| Average GM/GS grade | 13.1 | 13.1 | 0.0 |
| Average GM/GS salary | $137 | $144 | $7 |
| Average salary, Commissioned Corps (42 U.S.C. 207) | $146 | $153 | $7 |
| Average salary of ungraded positions | $202 | $212 | $10 |
| OBJECT CLASSES | FY 2023 Enacted | FY 2024 President’s Budget | FY 2024 +/- FY 2023 |
|---|---|---|---|
| Personnel Compensation | |||
| 11.1 Full-Time Permanent | $9,814 | $10,670 | $855 |
| 11.3 Other Than Full-Time Permanent | $2,509 | $2,772 | $263 |
| 11.5 Other Personnel Compensation | $787 | $863 | $76 |
| 11.7 Military Personnel | $216 | $247 | $31 |
| 11.8 Special Personnel Services Payments | $1,191 | $1,362 | $172 |
| 11.9 Subtotal Personnel Compensation | $14,516 | $15,913 | $1,397 |
| 12.1 Civilian Personnel Benefits | $5,325 | $5,784 | $459 |
| 12.2 Military Personnel Benefits | $19 | $21 | $3 |
| 13.0 Benefits to Former Personnel | $0 | $0 | $0 |
| Subtotal Pay Costs | $19,860 | $21,718 | $1,858 |
| 21.0 Travel & Transportation of Persons | $304 | $311 | $7 |
| 22.0 Transportation of Things | $10 | $10 | $0 |
| 23.1 Rental Payments to GSA | $0 | $0 | $0 |
| 23.2 Rental Payments to Others | $0 | $0 | $0 |
| 23.3 Communications, Utilities & Misc. Charges | $14 | $15 | $0 |
| 24.0 Printing & Reproduction | $0 | $0 | $0 |
| 25.1 Consulting Services | $6,155 | $4,999 | -$1,156 |
| 25.2 Other Services | $1,860 | $1,905 | $45 |
| 25.3 Purchase of goods and services from Government Accounts | $14,962 | $15,175 | $213 |
| 25.4 Operation & Maintenance of Facilities | $0 | $0 | $0 |
| 25.5 R&D Contracts | $6,361 | $6,442 | $81 |
| 25.6 Medical Care | $0 | $0 | $0 |
| 25.7 Operation & Maintenance of Equipment | $0 | $0 | $0 |
| 25.8 Subsistence & Support of Persons | $0 | $0 | $0 |
| 25.0 Subtotal Other Contractual Services | $29,338 | $28,520 | -$817 |
| 26.0 Supplies & Materials | $397 | $406 | $10 |
| 31.0 Equipment | $244 | $250 | $6 |
| 32.0 Land and Structures | $0 | $0 | $0 |
| 33.0 Investments & Loans | $0 | $0 | $0 |
| 41.0 Grants, Subsidies & Contributions | $120,111 | $119,046 | -$1,064 |
| 42.0 Insurance Claims & Indemnities | $0 | $0 | $0 |
| 43.0 Interest & Dividends | $0 | $0 | $0 |
| 44.0 Refunds | $0 | $0 | $0 |
| Subtotal Non-Pay Costs | $150,417 | $148,559 | -$1,858 |
| Total Budget Authority by Object Class | $170,277 | $170,277 | $0 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2023 Enacted | FY 2024 President’s Budget | FY 2024 +/- FY 2023 |
|---|---|---|---|
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $9,814 | $10,670 | $855 |
| Other Than Full-Time Permanent (11.3) | $2,509 | $2,772 | $263 |
| Other Personnel Compensation (11.5) | $787 | $863 | $76 |
| Military Personnel (11.7) | $216 | $247 | $31 |
| Special Personnel Services Payments (11.8) | $1,191 | $1,362 | $172 |
| Subtotal Personnel Compensation (11.9) | $14,516 | $15,913 | $1,397 |
| Civilian Personnel Benefits (12.1) | $5,325 | $5,784 | $459 |
| Military Personnel Benefits (12.2) | $19 | $21 | $3 |
| Benefits to Former Personnel (13.0) | $0 | $0 | $0 |
| Subtotal Pay Costs | $19,860 | $21,718 | $1,858 |
| Travel & Transportation of Persons (21.0) | $304 | $311 | $7 |
| Transportation of Things (22.0) | $10 | $10 | $0 |
| Rental Payments to Others (23.2) | $0 | $0 | $0 |
| Communications, Utilities & Misc. Charges (23.3) | $14 | $15 | $0 |
| Printing & Reproduction (24.0) | $0 | $0 | $0 |
| Other Contractual Services: | |||
| Consultant Services (25.1) | $6,155 | $4,999 | -$1,156 |
| Other Services (25.2) | $1,860 | $1,905 | $45 |
| Purchases of Goods and Services from Government Accounts (25.3) | $10,681 | $10,894 | $213 |
| Operation & Maintenance of Facilities (25.4) | $0 | $0 | $0 |
| Operation & Maintenance of Equipment (25.7) | $0 | $0 | $0 |
| Subsistence & Support of Persons (25.8) | $0 | $0 | $0 |
| Subtotal Other Contractual Services | $18,696 | $17,797 | -$899 |
| Supplies & Materials (26.0) | $397 | $406 | $10 |
| Subtotal Non-Pay Costs | $19,421 | $18,539 | -$881 |
| Total Administrative Costs | $39,280 | $40,258 | $977 |
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Full-Time Equivalent Employment (FTE)
| OFFICE | FY 2022 Final | FY 2023 Enacted | FY 2024 President’s Budget | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of Extramural Activities | |||||||||
| Direct: | 7 | - | 7 | 7 | - | 7 | 7 | - | 7 |
| Total: | 7 | - | 7 | 7 | - | 7 | 7 | - | 7 |
| Office of the Director | |||||||||
| Direct: | 6 | - | 6 | 5 | - | 5 | 5 | - | 5 |
| Total: | 6 | - | 6 | 5 | - | 5 | 5 | - | 5 |
| Office of Administrative Operations | |||||||||
| Direct: | 19 | - | 19 | 22 | - | 22 | 23 | - | 23 |
| Total: | 19 | - | 19 | 22 | - | 22 | 23 | - | 23 |
| Office of Policy, Planning, and Evaluation | |||||||||
| Direct: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Total: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Office of Communications and Public Liaison | |||||||||
| Direct: | 9 | - | 9 | 10 | - | 10 | 12 | - | 12 |
| Total: | 9 | - | 9 | 10 | - | 10 | 12 | - | 12 |
| Office of Clinical and Regulatory Affairs | |||||||||
| Direct: | 4 | - | 4 | 8 | - | 8 | 8 | - | 8 |
| Total: | 4 | - | 4 | 8 | - | 8 | 8 | - | 8 |
| Division of Extramural Research | |||||||||
| Direct: | 17 | - | 17 | 19 | - | 19 | 21 | - | 21 |
| Reimbursable: | 2 | - | 2 | 2 | - | 2 | 2 | - | 2 |
| Total: | 19 | - | 19 | 21 | - | 21 | 23 | - | 23 |
| Division of Intramural Research Program | |||||||||
| Direct: | 11 | 1 | 12 | 14 | 1 | 15 | 19 | 1 | 20 |
| Total: | 11 | 1 | 12 | 14 | 1 | 15 | 19 | 1 | 20 |
| Office of Scientific Review | |||||||||
| Direct: | 3 | - | 3 | 5 | - | 5 | 5 | - | 5 |
| Total: | 3 | - | 3 | 5 | - | 5 | 5 | - | 5 |
| Office of Grants Management | |||||||||
| Direct: | 4 | - | 4 | 4 | - | 4 | 4 | - | 4 |
| Total: | 4 | - | 4 | 4 | - | 4 | 4 | - | 4 |
| Total | 85 | 1 | 86 | 99 | 1 | 100 | 109 | 1 | 110 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| FISCAL YEAR | Average GS Grade | ||||||||
| 2020 | 13.3 | ||||||||
| 2021 | 13.2 | ||||||||
| 2022 | 13.1 | ||||||||
| 2023 | 13.1 | ||||||||
| 2024 | 13.1 | ||||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Positions1
| GRADE | FY 2022 Final | FY 2023 Enacted | FY 2024 President’s Budget |
|---|---|---|---|
| Total, ES Positions | 13 | 13 | 13 |
| Total, ES Salary | $2,600 | $2,799 | $2,799 |
| General Schedule | |||
| GM/GS-15 | 15 | 20 | 21 |
| GM/GS-14 | 17 | 18 | 20 |
| GM/GS-13 | 25 | 28 | 30 |
| GS-12 | 16 | 21 | 23 |
| GS-11 | 3 | 3 | 5 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 2 | 2 | 3 |
| GS-8 | 0 | 0 | 0 |
| GS-7 | 2 | 2 | 2 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 0 | 0 | 0 |
| GS-3 | 0 | 0 | 0 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 80 | 94 | 104 |
| Commissioned Corps (42 U.S.C. 207) | |||
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 1 | 1 | 1 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 1 | 1 | 1 |
| Ungraded | 10 | 10 | 10 |
| Total permanent positions | 78 | 88 | 98 |
| Total positions, end of year | 104 | 118 | 128 |
| Total full-time equivalent (FTE) employment, end of year | 86 | 100 | 110 |
| Average ES salary | $200 | $215 | $215 |
| Average GM/GS grade | 13.1 | 13.1 | 13.1 |
| Average GM/GS salary | $129,130 | $136,975 | $143,550 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||