Congressional Justification FY 2019
DEPARTMENT OF HEALTH AND HUMAN SERVICES
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health (NCCIH)
On this page:
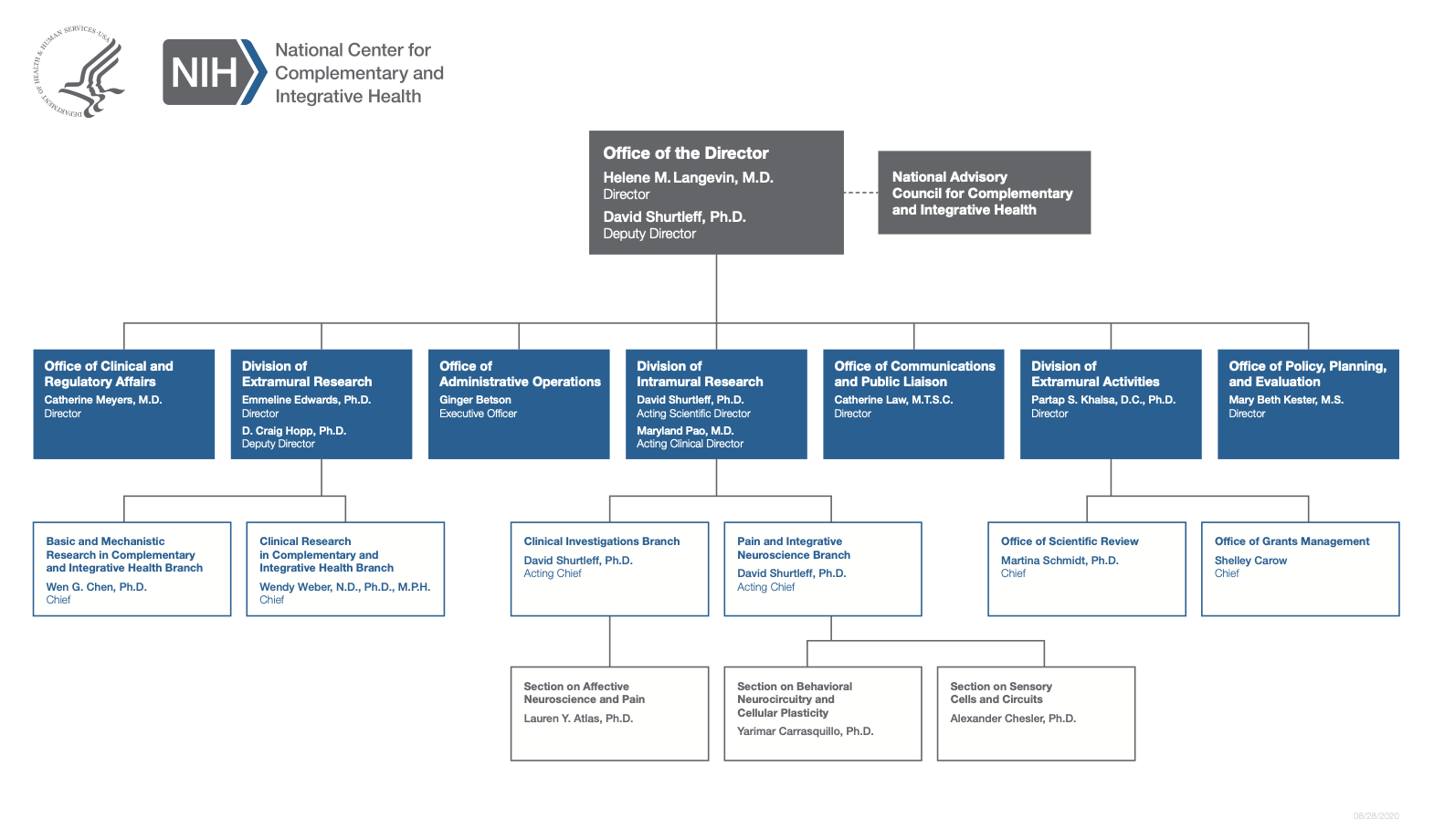
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Graphs
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
For carrying out section 301 and title IV of the PHS Act with respect to complementary and integrative health, $130,717,000.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Amounts Available for Obligation 1
(Dollars in Thousands)
| Source of Funding | FY 2017 Final | FY 2018 Annualized CR | FY 2019 President’s Budget |
|---|---|---|---|
| Appropriation | $134,689 | $134,689 | $130,717 |
| Mandatory Appropriation: (non-add) | |||
| Type 1 Diabetes | (0) | (0) | (0) |
| Other Mandatory financing | (0) | (0) | (0) |
| Rescission | 0 | -915 | 0 |
| Sequestration | 0 | 0 | 0 |
| Secretary's Transfer | -300 | ||
| Subtotal, adjusted appropriation | $134,389 | $133,774 | $130,717 |
| OAR HIV/AIDS Transfers | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $134,389 | $133,774 | $130,717 |
| Unobligated balance, start of year | 0 | 0 | 0 |
| Unobligated balance, end of year | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $134,389 | $133,774 | $130,717 |
| Unobligated balance lapsing | -16 | 0 | 0 |
| Total obligations | $134,389 | $133,774 | $130,717 |
| 1 Excludes the following amounts for reimbursable activities carried out by this account: FY 2017 — $564 FY 2018 — $460 FY 2019 — $460 | |||
Fiscal Year 2019 Budget Graphs
History of Budget Authority and FTEs:
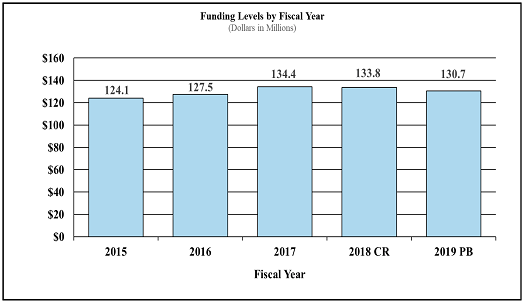
Funding Levels by Fiscal Year
| Fiscal Year | Dollars in Millions |
|---|---|
| 2015 | $124.1 |
| 2016 | $127.5 |
| 2017 | $134.4 |
| 2018 | $133.8 |
| 2019 | $130.7 |
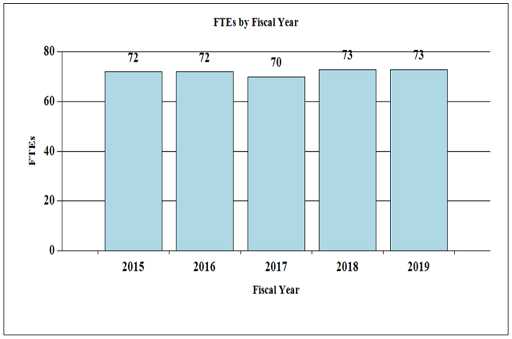
Full-Time Employees by Fiscal Year
| FY | FTEs |
|---|---|
| 2015 | 72 |
| 2016 | 72 |
| 2017 | 70 |
| 2018 | 73 |
| 2019 | 73 |
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2018 Amount Authorized | FY 2018 Annualized CR | 2019 Amount Authorized | FY 2019 President’s Budget | |||
|---|---|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | Indefinite | ||||
| $133,774,327 | $130,717,000 | |||||||
| National Center for Complementary and Integrative Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total, Budget Authority | $133,774,327 | $130,717,000 | ||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation | ||||
|---|---|---|---|---|---|---|---|---|
1 Budget Estimate to Congress includes mandatory financing. | ||||||||
| 2009 | $121,695,000 | $125,878,000 | $125,082,000 | $125,471,000 | ||||
| Rescission | $0 | |||||||
| 2010 | $127,241,000 | $129,953,000 | $127,591,000 | $128,844,000 | ||||
| Rescission | $0 | |||||||
| 2011 | $132,004,000 | $131,796,000 | $128,844,000 | |||||
| Rescission | $1,131,327 | |||||||
| 2012 | $131,002,000 | $131,002,000 | $126,275,000 | $128,299,000 | ||||
| Rescission | $242,485 | |||||||
| 2013 | $127,930,000 | $128,318,000 | $128,056,515 | |||||
| Rescission | $256,113 | |||||||
| Sequestration | ($6,427,556) | |||||||
| 2014 | $129,041,000 | $128,183,000 | $124,296,000 | |||||
| Rescission | $0 | |||||||
| 2015 | $124,509,000 | $124,681,000 | ||||||
| Rescission | $0 | |||||||
| 2016 | $127,521,000 | $127,585,000 | $130,162,000 | $130,789,000 | ||||
| Rescission | $0 | |||||||
| 20171 | $129,941,000 | $134,549,000 | $136,195,000 | $134,689,000 | ||||
| Rescission | $0 | |||||||
| 2018 | $101,793,000 | $136,741,000 | $139,654,000 | $134,689,000 | ||||
| Rescission | $914,673 | |||||||
| 2019 | $130,717,000 | |||||||
Justification of Budget Request
National Center for Complementary and Integrative Health
Authorizing Legislation: Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2017 Actual | FY 2018 Annualized CR | FY 2019 President’s Budget | FY 2019 +/- FY 2018 | |
|---|---|---|---|---|
| BA | $134,389,000 | $133,774,327 | $130,717,000 | -$3,057,327 |
| FTE | 70 | 73 | 73 | 0 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Director's Overview
The National Center for Complementary and Integrative Health (NCCIH) is the lead Federal agency for scientific research on the safety and efficacy of complementary and integrative health practices. These practices range from the use of natural products (e.g., dietary supplements, probiotics, and botanicals) to mind and body interventions (e.g., meditation, yoga, cognitive-behavioral therapy, acupuncture, spinal manipulation, and massage). Recent analysis of the 2012 National Health Interview Survey (NHIS) found that Americans spend approximately $30.2 billion a year on complementary approaches. 1 They utilize these treatments to improve health, manage symptoms of chronic diseases, and/or counter the side effects of conventional medicine. NCCIH is committed to providing the American public with information about these practices that is based on rigorous scientific investigation.
NCCIH strives to invest in research that will drive new discoveries, which may lead to improved public health and health care. The Center focuses on areas with the greatest potential impact by prioritizing research topics that are showing scientific promise and that are amenable to rigorous scientific inquiry. As a responsible steward of resources, NCCIH is highly selective in its support of a broad range of meritorious basic, clinical, and translational research. The Center also promotes the development of the next generation of complementary and integrative health scientists through training grants, travel awards, and career development workshops.
Exploring nonpharmacologic approaches for pain management
NCCIH supports rigorous basic research and clinical trials evaluating nonpharmacologic pain management approaches. Chronic pain is a major public health problem in the United States, especially within military and veteran populations. Opioids, which are highly addictive, are often prescribed to treat chronic pain. As a result, the United States faces a growing opioid misuse epidemic necessitating the development of new pain management strategies. NCCIH is devoting significant resources to understand the basis of pain and whether complementary and integrative health approaches can be utilized in pain management.
NCCIH-funded research has provided insight into how pain is transmitted and interpreted by the body. Recently, scientists discovered a new class of sensory nerve cells that respond to high-threshold (intense) mechanical stimuli, such as hair pulling. 2 This work provides insights into how our bodies encode and transmit pain sensations. Another study co-funded by NCCIH mapped the regions of the brain activated during pain to establish a “pain signature.” This study found that specific regions of the brain respond to pain intensity, while other regions mediate the psychological effect, and yet another region showed increased activity related to pain relief. 3 This work not only provides insights into how pain is interpreted, but could lead to the development of new methods to detect, quantify, or target pain.
NCCIH-supported research evaluates the benefits of mind and body approaches as an integrative pain management strategy. One study investigated the effect of acupuncture on carpal tunnel syndrome and found that it improved function and nerve conduction, decreased associated pain, and affected activity of pain centers in the brain. 4 Another study mapped the impact of mindfulness meditation on brain activity and found that it activates the same region of the brain as opioids; however, it reduces pain independently of opioid neurotransmitter mechanisms. These results suggest that greater pain control could be achieved through the combination of mindfulness meditation and pharmacologic or nonpharmacologic approaches that involve opioid signaling. 5 These results and others supported by the NCCIH led to the formation of a new multi-agency partnership led by NCCIH, with participation by NIAAA, NICHD, NIDA, NINDS, NINR, OBSSR, and the NIH ORWH, as well as the Department of Defense and Department of Veterans Affairs, to study nondrug approaches for pain management within the military and veteran health care systems (see Program Portrait).
- Nahin RL, Barnes PM, Stussman BJ. Expenditures on complementary health approaches: United States, 2012. National Health Statistics Reports; no. 95, 2016. PMID: 2735222.
- Ghitani N, et al. Specialized mechanosensory nociceptors mediating rapid responses to hair-pull. Neuron. 2017; 95(4):944-954.e4. PMID: 28817806.
- Woo C-W, et al. Quantifying cerebral contributions to pain beyond nociception. Nature Communications. 2017; 8:14211. PMID: 28195170.
- Maeda Y, et al. Rewiring the primary somatosensory cortex in carpal tunnel syndrome with acupuncture. Brain. 2017; 140(4):914-927. PMID: 28334999.
- Zeidan F, et al. Mindfulness-meditation-based pain relief is not mediated by endogenous opioids. Journal of Neuroscience. 2016; 36(11):3391-3397. PMID: 26985045.
Advancing research on natural products
NCCIH continues to support rigorous research on promising natural products. The Center strives to fund the development and pilot-testing of natural products currently used by many adults and children. NCCIH funds research on the risks, mechanism of action, and potential clinical benefit of these natural products. The Center seeks to streamline natural product clinical research through a phased research pipeline starting with early phase studies exploring the mechanism of action. The most promising natural products will advance to the later research phases that support investigations comparing clinical outcomes and biological effects through randomized controlled efficacy trials. In FY 2017, NCCIH released two funding opportunity announcements to solicit grant applications in these areas. NCCIH and the NIH Office of Dietary Supplements are also funding two Centers for Advancing Natural Products Innovation and Technology to develop pioneering methods and techniques to catalyze new research approaches and technologies that may have significant impact on the chemical and biological investigation of natural products.
NCCIH also currently supports research on cytisine, a natural product for smoking cessation. Cytisine, isolated more than 50 years ago from the plant Laburnum anagyroides, binds to the same receptors as nicotine, and has been used as a smoking cessation aid, primarily in several eastern European countries, for several decades. Despite promising results from clinical trials conducted outside the United States, cytisine has not yet been approved for use in the United States. NCCIH supported a series of pre-clinical studies on cytisine through a strategic collaboration with Achieve Life Sciences, Inc., OncoGenex Pharmaceutical, Inc., other NIH ICs, and private research organizations. Recently, the FDA allowed an Investigational New Drug application to go into effect that permits phase 2 clinical studies to further assess cytisine as a smoking cessation treatment. This continuing public-private partnership may lead to the wide availability of a new smoking cessation option to address the major public health issues associated with tobacco use.
Program Descriptions and Accomplishments
Extramural Clinical Research:
The NCCIH extramural research program funds clinical investigations on complementary and integrative health practices and interventions. Projects range from small pilot studies to large-scale clinical trials and epidemiologic studies, including several collaborations between NIH ICs and other Federal agencies. For example, recent results from an NCCIH-supported study, published in the Annals of Internal Medicine, showed that yoga and physical therapy offer similar pain relief and functional benefits to a racially diverse group of participants with low socioeconomic status who had chronic low back pain. These findings suggest that a structured yoga program may be an alternative to physical therapy for people with chronic low back pain, depending on individual preferences, availability, and cost. 6
Program Portrait – Joint NIH-DoD-VA Pain Management Collaboratory
Pain is the most common medical condition requiring treatment for military personnel. Studies report nearly 45 percent of soldiers and 50 percent of veteran’s experience pain on a regular basis, and there is significant overlap among chronic pain, post-traumatic stress disorder (PTSD), and persistent post-concussive symptoms. Data from the 2010-2014 National Health Interview Survey shows that American veterans experience a higher prevalence of pain and more severe pain than non-veterans. 7 Although opioids are often prescribed to treat chronic pain, there is no evidence to suggest that they are effective. Furthermore, they frequently are associated with severe adverse effects and may lead to drug addiction. 8 Therefore, there is a need for nondrug approaches to complement current strategies for pain management and to reduce the need for, and hazards of, excessive reliance on opioids.
The NCCIH is leading an interagency partnership involving the U.S. Department of Health and Human Services (HHS), the U.S. Department of Defense (DoD), and the U.S. Department of Veterans Affairs (VA) to fund a multi-project research program focusing on nondrug approaches for pain management. This initiative, called the NIH DoD-VA Pain Management Collaboratory, will focus on developing, implementing, and testing cost-effective, large-scale, real-world research on nondrug approaches for pain management and related conditions in military and veteran health care delivery organizations. The Collaboratory plans to fund twelve research projects, totaling approximately $81 million over six years, with the NCCIH contributing more than half of these funds. In spite of limited resources, this program will remain a high priority for the NCCIH. The research projects will provide valuable information about the feasibility, acceptability, safety, and effectiveness of nondrug approaches in treating pain within health care systems. Types of approaches being studied include mindfulness/meditative interventions, movement interventions (e.g., structured exercise, tai chi, yoga), manual therapies (e.g., spinal manipulation, massage, acupuncture), psychological and behavioral interventions (e.g., cognitive behavioral therapy), integrative approaches that involve more than one intervention, and integrated models of multi-modal care. The results of these studies may inform new pain management practices within the DoD and VA and support the use of nondrug approaches for pain management in the general population.
- Saper RB, et al. Yoga, physical therapy, or education for chronic low back pain: a randomized noninferiority trial. Annals of Internal Medicine. 2017 Jul 18;167(2):85-94. PMID: 28631003.
- Nahin RL. Severe pain in veterans: the impact of age and sex, and comparisons to the general population. Journal of Pain. 2017; 18(3):247-254. PMID: 27884688.
- Chou R, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015 Feb 17;162(4):276-86. PMID: 25581257.
Extramural Basic Research
Basic research on the fundamental biological effects of active components of interventions is central to the development of the evidence base on complementary and integrative health approaches and underpins the design of clinical research. While NCCIH continues its broad support of investigator-initiated research, the Center will also support translational research to optimize therapeutic effects through targeted initiatives. For example, NCCIH supports translational research to ascertain the biological effects of nonpharmacologic therapies on the brain and to optimize their effects. NCCIH also is energizing the research community to overcome the methodologic and technologic obstacles hindering basic research on natural products and nonpharmacologic therapies, as well as encouraging the incorporation of cutting-edge technologies to monitor and enhance these interventions.
Extramural Research Training and Capacity Building
Improving the capacity of the field to carry out rigorous research on complementary and integrative health approaches is a priority for NCCIH. To increase the number, quality, and diversity of investigators conducting research on complementary and integrative health approaches, NCCIH supports a variety of training and career development activities for pre- and post-doctoral students, and early career investigators. In October 2017, the NCCIH held a two day workshop for its supported fellows and trainees to assist them in eventually becoming independent researchers. Sessions included information on NCCIH funding opportunities across the stages of career development, NCCIH research priorities, successfully navigating the NIH peer review process, choosing a mentor, becoming an early stage investigator, and crafting a career development grant proposal. It is anticipated that the Center will continue to conduct this workshop every other year to cultivate the next generation of researchers in complementary and integrative health.
Intramural Research
NCCIH’s intramural research program is focused on understanding the central mechanisms of pain and its modulation, with the long-term goal of improving clinical management of chronic pain through the integration of pharmacologic and nonpharmacologic approaches. Among topics of interest are the pathways and mechanisms by which expectations, emotions, attention, environment, and genetics modulate pain or pain processing. The program both engages and leverages the exceptional basic and clinical research talent and resources of other neuroscience and neuroimaging efforts within the NIH intramural community.
Research Management and Support (RMS)
Through its RMS activities, NCCIH provides administrative, budgetary, logistical, and scientific support in the review, award, monitoring, and management of research grants, training awards, and contracts. The Center has recently begun utilizing QlikView, a business intelligence enterprise solution, to provide NCCIH leadership with a comprehensive view of trends, anomalies, and performance indicators to ensure responsible stewardship of public funds. NCCIH is also improving its onboarding process by creating a toolkit to standardize the material given to new employees. As part of its outreach efforts, NCCIH disseminates objective, evidence-based information to the public, scientists, and health care providers to help them make informed decisions about the use of complementary and integrative health practices.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Full-Time Equivalent Employment (FTE)
| OFFICE/DIVISION | FY 2017 Final | FY 2018 Annualized CR | FY 2019 President’s Budget | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Office of Scientific Review | |||||||||
| Direct: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Basic and Mechanistic Research in Complementary and Integravtive Health Branch | |||||||||
| Direct: | 1 | - | 1 | 2 | - | 2 | 2 | - | 2 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 1 | - | 1 | 2 | - | 2 | 2 | - | 2 |
| Clinical Research in Complementary and Integrative Health Branch | |||||||||
| Direct: | 4 | - | 4 | 4 | - | 4 | 4 | - | 4 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 4 | - | 4 | 4 | - | 4 | 4 | - | 4 |
| Division of Extramural Activities | |||||||||
| Direct: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Division of Extramural Research | |||||||||
| Direct: | 7 | - | 7 | 8 | - | 8 | 8 | - | 8 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 7 | - | 7 | 8 | - | 8 | 8 | - | 8 |
| Divison of Intarmural Research Program | |||||||||
| Direct: | 6 | 2 | 8 | 7 | 2 | 9 | 7 | 2 | 9 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 6 | 2 | 8 | 7 | 2 | 9 | 7 | 2 | 9 |
| Office of Administrative Operations | |||||||||
| Direct: | 16 | - | 16 | 16 | - | 16 | 16 | - | 16 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 16 | - | 16 | 16 | - | 16 | 16 | - | 16 |
| Office of Clinical and Regulatory Affairs | |||||||||
| Direct: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Office of Communications and Public Liaison | |||||||||
| Direct: | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 |
| Office of Grants Management | |||||||||
| Direct: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Office of Policy, Planning and Evaluation | |||||||||
| Direct: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Office of the Director | |||||||||
| Direct: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 5 | - | 5 | 5 | - | 5 | 5 | - | 5 |
| Total | 68 | 2 | 70 | 71 | 2 | 73 | 71 | 2 | 73 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| FISCAL YEAR | Average GS Grade | ||||||||
| 2015 | 12.6 | ||||||||
| 2016 | 12.8 | ||||||||
| 2017 | 12.9 | ||||||||
| 2018 | 12.9 | ||||||||
| 2019 | 12.9 | ||||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Positions1
| GRADE | FY 2017 Final | FY 2018 Annualized CR | FY 2019 President’s Budget |
|---|---|---|---|
| Total, ES Positions | 0 | 0 | 0 |
| Total, ES Salary | 0 | 0 | 0 |
| GM/GS-15 | 8 | 8 | 8 |
| GM/GS-14 | 14 | 14 | 14 |
| GM/GS-13 | 18 | 19 | 19 |
| GS-12 | 8 | 9 | 9 |
| GS-11 | 5 | 5 | 5 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 0 | 0 | 0 |
| GS-8 | 1 | 1 | 1 |
| GS-7 | 2 | 2 | 2 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 0 | 0 | 0 |
| GS-3 | 0 | 0 | 0 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 56 | 58 | 58 |
| Grades established by Act of July 1, 1944 (42 U.S.C. 207) | 0 | 0 | 0 |
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 1 | 1 | 1 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 1 | 1 | 1 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 2 | 2 | 2 |
| Ungraded | 9 | 10 | 10 |
| Total permanent positions | 58 | 61 | 61 |
| Total positions, end of year | 67 | 70 | 70 |
| Total full-time equivalent (FTE) employment, end of year | 70 | 73 | 73 |
| Average ES salary | 0 | 0 | 0 |
| Average GM/GS grade | 12.9 | 12.9 | 12.9 |
| Average GM/GS salary | 114,460 | 116,635 | 117,189 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||